What Is Diabetic Retinopathy?
Diabetic retinopathy, also called DR, is a complication of diabetes (type 1 or 2) that injures the retina, a tissue in the back of the eye. Elevated blood sugar from diabetes damages the blood vessels and light sensitive parts of the retina. It is possible to have diabetic retinopathy without any symptoms. It is also possible for symptoms to appear and then resolve. Dilated eye exams are important for people with and without symptoms.1-3
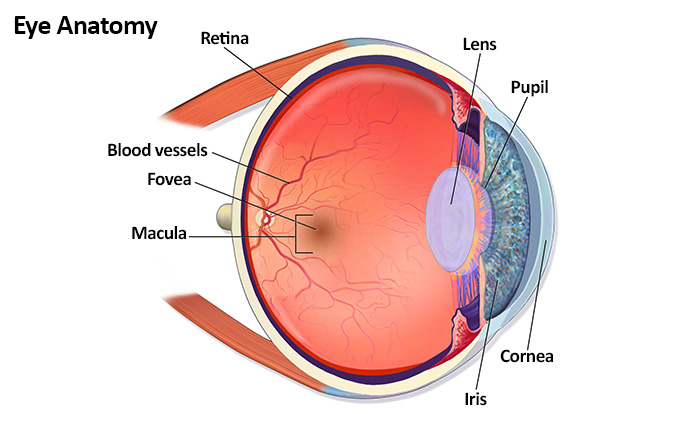
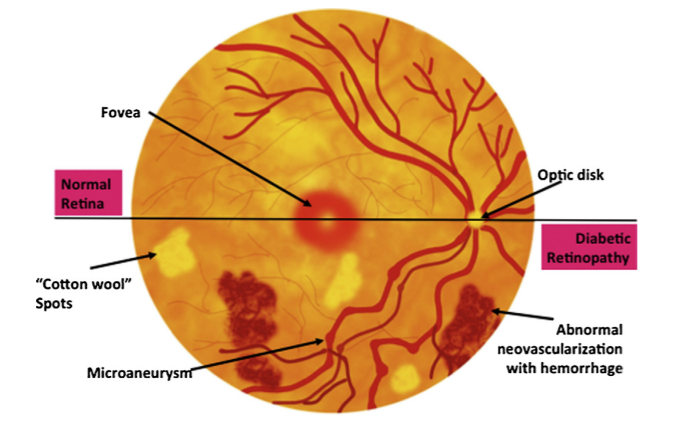
The eye is a very complicated organ — although a small organ, there are many parts of the eye that allow us to see. Some terms that will help you understand some of the information about diabetic retinopathy are listed below.4-6
- Fovea: Small depression in the retina where central vision sharpness is highest. The fovea is located within the center of the macula.
- Fundus: The inside, back surface of the eye, which is made up of the retina, macula, optic disc, fovea, and blood vessels
- Intravitreal injection: Form of treatment for diabetic retinopathy in which a medication is injected into the vitreous cavity in the middle of the eye
- Macula: A small area at the center of the retina, which is responsible for central (straight-ahead) vision, the majority of color vision, and the ability to see small details
- Neovascularization: New blood vessels that grow uncontrollably, provoked by a lack of oxygen, which can cause vision loss
- Proliferative diabetic retinopathy (PDR): An advanced stage of diabetic retinopathy in which new abnormal blood vessels and scar tissue form on the surface of the retina; scar tissue can pull on the retina, which can cause retinal detachment and loss of vision
- Retina: Thin layer of nerve tissue that lines the back of the eye; it receives and converts light into electrical signals, which are then sent to the brain by the optic nerve, resulting in sight
- Vitreous: A gel-like substance that fills the inside of the eyeball
Diabetic retinopathy is the most common cause of new cases of nonhereditary blindness in the US among adults aged 18 to 65 years, and strongly correlates to both the duration of diabetes and how well blood sugar is controlled.8-11 In the US, diabetic retinopathy affects approximately 86% of patients with type 1 diabetes mellitus (T1DM) and 40% of patients with type 2 diabetes mellitus (T2DM).12-14 According to the Centers for Disease Control and Prevention (CDC), nearly 22% of the 4.1 million Americans with diabetic retinopathy are at risk for complications that can threaten vision.13
Vision loss due to diabetic retinopathy can occur through a variety of pathways, highlighted in the following Figure.15
- Central vision may be affected by swelling in the macula (called macular edema), which can blur and distort images, making them more difficult to see clearly. This swelling is usually caused by fluid leaking from either damaged blood vessels or new, fragile (neovascular) blood vessels into the layers of the macula.16
- Continued damage to the small blood vessels of the retina can decrease blood circulation and cause new, abnormal blood vessels as well as scar tissue to grow on the surface of the retina. This is known as proliferative diabetic retinopathy (PDR).17
- These new, abnormal (neovascular) blood vessels may bleed into the middle of the eye, or may grow on the iris, clogging the drainage system of the eye, both of which can cause vision loss.17
- Scar tissue can pull on the retina and cause the retina to detach from the back of the eye, causing vision loss.17
Macular edema can occur at any stage of diabetic retinopathy and is one of the most common causes of visual loss in patients with diabetes mellitus.18 If left untreated, continued (chronic) macular edema can lead to irreversible damage to the macula and permanent vision loss.16
References
- Abcouwe SF, Gardner TW. Diabetic retinopathy: loss of neuroretinal adaptation to the diabetic metabolic environment. Ann N Y Acad Sci. 2014;1311:174-190.
- Shah AR, Garder TW. Diabetic retinopathy: research to clinical practice. Clin Diabetes Endocrinol. 2017;3:9.
- Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic Retinopathy Preferred Practice Pattern. Ophthalmology. 2020;127(1):PP66-PP145.
- American Society of Retina Specialists (ASRS). Diabetic retinopathy. https://www.asrs.org/patients/retinal-diseases/3/diabeticretinopathy. Accessed January 12, 2022.
- Turbert D. American Academy of Ophthalmology (AAO). Fundus. 2020. https://www.aao.org/eye-health/anatomy/fundus. Accessed January 12, 2022.
- Macular Society. What is the macula? 2022. https://www.macularsociety.org/macular-disease/macula/. Accessed January 12, 2022.
- Blausen.com staff. Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1. 2014. https://commons.wikimedia.org/wiki/File:Blausen_0389_EyeAnatomy_02.png. Accessed January 12, 2022.
- Farley TM, Mandava N, Prall FR, Carsky C. Accuracy of primary care clinicians in screening for diabetic retinopathy using single-image retinal photography. Ann Fam Med. 2008;6:428-434.
- Varma R. Diabetic retinopathy: challenges and future directions. Am J Ophthalmol. 2006;141:539-541.
- Solomon SD, Chew E, Duh EJ, et al. Diabetic retinopathy: a position statement by the American
Diabetes Association. Diabetes Care. 2017;40(3):412-418. - Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2020.
- CDC Vision Health Initiative. Diabetic retinopathy. https://www.cdc.gov/visionhealth/vehss/data/studies/diabetic-retinopathy.html.
- Opere CA, O’Brien KK, Shea JL. Understanding diabetic retinopathy. US Pharm. 2011;36:46-52.
- Cheung N, Mitchell P, Wong T. Diabetic retinopathy. 2010;376:124-136.
- Eshaq RS, Aldalati AMZ, Alexander JS, Harris NR. Diabetic retinopathy: breaking the barrier. Pathophysiology. 2017;24:229-241.
- ASRS. Retinal Health Series. Macular edema. 2022. https://www.asrs.org/patients/retinal-diseases/20/macular-edema. Accessed January 12, 2022.
- ASRS. Retinal Health Series. Diabetic retinopathy. 2022. https://www.asrs.org/patients/retinal-diseases/3/diabetic-retinopathy. Accessed January 12, 2022.
- Javey G, Schwartz SG, Flynn Jr HW. Emerging pharmacotherapies for diabetic macular edema. Exp Diabetes Res.
2012;2012(548732):1-12.